Past Issues
Thermal Burns in Newborns at the Mother and Child University Hospital Center of Ndjamena, Chad
Olivier Ngaringuem*, Mahamat Nour Abakar Djibrine, Bembo Lamega, Kalki Ndjiannone, Hortebaye
Mother and Child Hospital of N'Djamena, University of N'Djamena, Chad
*Corresponding author: Dr. Olivier Ngaringuem, Mother and Child Hospital of N'Djamena, University of N'Djamena, Chad, Phone: 91642011, E-mail: [email protected]
Received Date: May 29, 2025
Published Date: July 10, 2025
Citation: Ngaringuem O, et al. (2025). Thermal Burns in Newborns at the Mother and Child University Hospital Center of Ndjamena, Chad. Neonatal. 6(1):25.
Copyrights: Ngaringuem O, et al. © (2025).
ABSTRACT
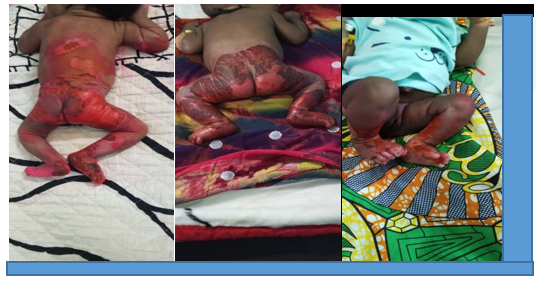
Introduction: Burns represent an acute and sometimes complete destruction of the skin barrier and constitute a significant public health issue among children. This study aims to characterize the epidemiological, etiological, clinical, and outcome-related features of thermal burns in newborns. Methodology: We conducted a descriptive cross-sectional study over a 12-month period, including all newborns admitted for thermal burn management in the burns unit of the pediatric surgery department at the Mother and Child University Hospital Center in Ndjamena. Variables analyzed included age, sex, circumstances and timing of the burn, type of burn, causative agent, extent and depth of injury, delay before medical care, pre-hospital interventions, associated injuries, in-hospital management, and clinical outcomes. Results are reported as frequencies and means. Results: Over the study period, pediatric burns accounted for 9.96% of all hospital admissions. Among these, there were 22 cases of neonatal burns, constituting 5.4% of all burn admissions to the department. Infants aged 0 to 7 days comprised 45.5% of these cases. Males accounted for 59.1% of cases, yielding a sex ratio of 1.7. All neonatal burns were caused by exposure to hot liquids, specifically bath water. A total of 95.5% of newborns were admitted to the emergency department within six hours of sustaining the burn injury. Newborns with burns covering 5 to 10% of their body surface area represented 54.5% of cases. Second-degree burns were observed in 95.5% of cases, while third-degree burns were present in 4.5%. The external genitalia and perineal region were affected in 68.2% of cases. Hospitalization lasting between 7 and 14 days occurred in 63.6% of cases. Favorable outcomes were achieved in 86.4% of cases. Conclusion: Thermal burns in the neonatal period are a significant concern in our clinical practice. These injuries are most often attributable to exposure to hot water during bathing, and are largely preventable. It is therefore imperative to educate parents of newborns on the use of lukewarm water for bathing.
Keywords: Burn, Thermal, Newborn, Pediatrics, Chad
INTRODUCTION
Burns are defined as an acute, and sometimes complete, destruction of the skin barrier caused by thermal, chemical, or electrical agents [1]. Globally, burns represent a significant public health challenge, accounting for over 310,000 deaths annually [2]. In sub-Saharan Africa, between 18,000 and 30,000 individuals under the age of 18 succumb to burns each year, making burns the second most common cause of accidental mortality among African children under five years old [3]. The severity of burns is recognized when the affected surface area exceeds 10% in children, 5% in those under one year of age, and any burn occurring during the neonatal period is considered severe by default. Severity is also influenced by burn depth (deep second-degree and third-degree burns), anatomical location (face, perineum, extremities, and joints), causative mechanism (electrical, chemical, or thermal), and the presence of associated injuries such as respiratory compromise [1,4,5].
In Chad, although several studies have examined pediatric burns in general, data specifically addressing thermal burns in the neonatal period remain scarce. Therefore, the present study was undertaken to describe the epidemiological, etiological, clinical, and outcome characteristics of thermal burns in neonates.
PATIENTS AND METHODS
A descriptive cross-sectional study was conducted over a 12-month period, from January 2023 to December 2023. The study population comprised neonates (aged from birth to 30 days) admitted for the management of thermal burns to the burn unit of the pediatric surgery department at the Mother and Child University Hospital Center in Ndjamena. Exclusion criteria were age beyond the neonatal period and lack of parental consent for participation. The variables analyzed included age, sex, circumstances and timing of the burn injury, type of burn, causative agent, extent and depth of the burn, time to initiation of care, pre-hospital management, associated injuries, in-hospital management, and clinical outcomes. Data were collected using a standardized form and entered into Microsoft Excel 2003. Results were expressed as frequencies and means.
RESULTS
Epidemiological Characteristics
Frequency
Over the course of the study period, a total of 4,036 patients were admitted to the pediatric surgery department, of whom 402 were hospitalized for burns. Consequently, burn cases accounted for 9.96% of all admissions. Among these, 22 cases involved newborns, constituting 5.4% of all burn-related admissions to the department.
Age Distribution of Newborns
Table 1. Distribution of newborns by age group
|
Age group |
n |
% |
|
0–7 days |
10 |
45.5 |
|
7–14 days |
8 |
36.3 |
|
14–29 days |
4 |
18.2 |
|
Total |
22 |
100.0 |
The 0–7 days age group accounted for 45.5% of the cases.
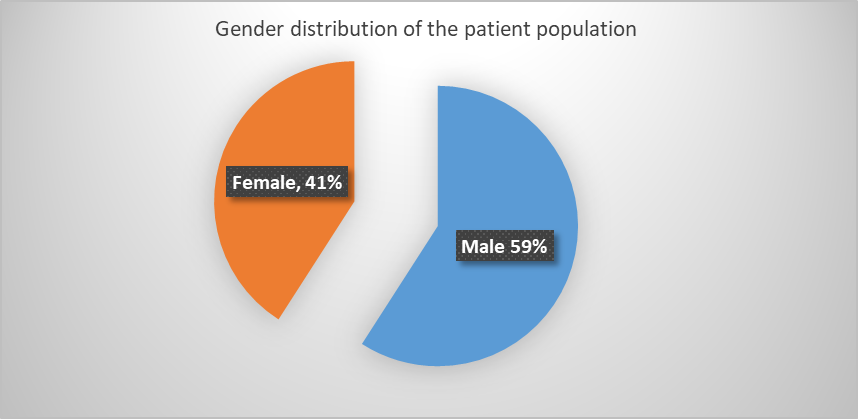
Sex
Figure 1. Distribution of patients by sex.
Male patients accounted for 59.1% of cases, yielding a sex ratio of 1.7.
Month of Admission
Table 2. Patient Distribution by Month of Admission
|
Month of Admission |
N |
% |
|
January |
3 |
13.6 |
|
Feburary |
3 |
13.6 |
|
March |
3 |
13.6 |
|
April |
1 |
4.5 |
|
May |
0 |
0.0 |
|
June |
2 |
9.1 |
|
July |
0 |
0.0 |
|
August |
2 |
9.1 |
|
September |
3 |
13.6 |
|
October |
2 |
9.1 |
|
November |
1 |
4.5 |
|
December |
2 |
9.1 |
|
Total |
22 |
100.0 |
CLINICAL DATA
Etiology of Burns
All neonates sustained burns caused by hot liquids (bath water).
Source
All neonates were admitted directly from home.
Time to Admission
Table 3. Distribution of patients according to time to admission
|
Time to Admission |
n |
% |
|
0 to 6 hours |
21 |
95.5 |
|
7 to 24 hours |
1 |
4.5 |
|
More than 24 hours |
0 |
0 |
|
Total |
22 |
100 |
Ninety-five point five percent of neonates were admitted to the emergency department within the first six hours after sustaining a burn.
Burned Body Surface Area
Table 4. Distribution of patients according to the extent of burned body surface area
|
Burned Body Surface Area |
n |
% |
|
0–5% |
1 |
4.5 |
|
5–10% |
8 |
36.3 |
|
10–15% |
12 |
54.5 |
|
More than 15% |
1 |
4.5 |
|
Total |
22 |
100.0 |
Newborns with a burned body surface area between 5% and 10% accounted for 54.5% of the cases.
Degree of Burn
Second-degree burns accounted for 95.5% of cases, while third-degree burns were observed in 4.5% of cases.
Burn Location
Table 5. Distribution of patients according to burn location
|
Burn Location |
N |
% |
|
Lower limb |
6 |
27.3 |
|
Abdomen |
0 |
0.0 |
|
External genitalia and perineum |
15 |
68.2 |
|
Head |
0 |
0.0 |
|
Thorax |
0 |
0.0 |
|
Lower limb and abdomen |
1 |
4.5 |
|
Abdomen and back |
0 |
0.0 |
|
Total |
22 |
100.0 |
Burns were localized to the external genitalia and perineal region in 68.2% of cases.
Hospitalization
Table 6. Distribution of patients by length of hospital stay
|
Hospital Stay |
n |
% |
|
Less than 7 Days |
4 |
18.2 |
|
7 to 14 Days |
14 |
63.6 |
|
15 Days to 1 Month |
4 |
18.2 |
|
Total |
22 |
100.0 |
A hospital stays of 7 to 14 days accounted for 63.6% of cases.
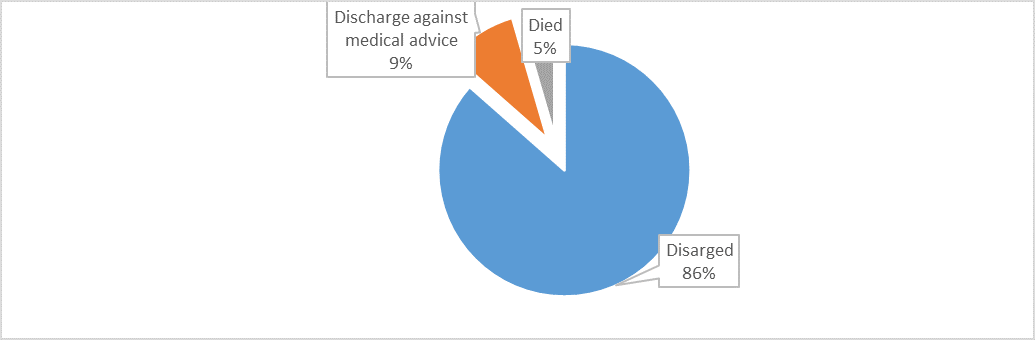
Evolution
Figure 2. Distribution of patients by outcome.
A favorable outcome was observed in 86.4% of cases.
DISCUSSION
The incidence of neonatal burns was 5.4%. These burns constitute an established reality in our setting and occur consistently throughout the year. This rate is comparable to those reported by some authors in sub-Saharan Africa [6,7], but exceeds the rate observed in Pakistan [8]. In other studies, the mean age was between 4 and 5 years, and burns among neonates were almost anecdotal [9,10]. In neonates, burns typically involve the full thickness of the skin due to thermal injury, whereas in older children, such injuries more often result in superficial or partial-thickness burns [11]. The majority of cases involved newborns aged 0 to 7 days. Maher et al. described a case involving a 16-day-old neonate [12], while Iqbal T. et al. reported a mean age of 11.18 ± 9.67 days [13]. The sex ratio was 1.7, with males accounting for 59.1% of cases. SAAIQ M. et al. also reported a predominance of male newborns (72.7%), corresponding to a sex ratio of 2.7 [11].
At the Mother and Child University Hospital Center in Ndjamena, the etiology of neonatal burns was exclusively attributed to exposure to hot water during newborn bathing. This phenomenon may be explained by the increased vulnerability of neonatal skin compared to that of older children [14]. In developed countries, a variety of iatrogenic mechanisms have been documented as causes of neonatal burns [15]. Across Africa, irrespective of age, scald injuries represent the most prevalent cause of burns [16]. In the local context, it appears that most families employ water that is nearly boiling for bathing infants. Culturally, it is believed that bathing neonates in very hot water promotes rapid physical and motor development. However, factors such as parental negligence and socioeconomic status may also contribute to accidental burn injuries.
The time to hospital admission for affected neonates did not exceed seven hours post-injury. This prompt presentation may be attributed to the ready accessibility of healthcare facilities and increased awareness regarding the severity of neonatal burn injuries, which are regarded as serious from the outset. In over half the cases, the total body surface area burned ranged between 10% and 15% as assessed by the Lund and Browder chart, with the majority of injuries classified as superficial second-degree burns. Reports on the percentage of total body surface area affected vary, likely reflecting differences in the quantity of the causative agent, duration of contact, and the inherent fragility of neonatal skin [17].
The most common sites of injury were the external genitalia, perineum, and lower limbs (15 cases, or 68.2%), with hospital stays ranging from 7 to a maximum of 14 days. These anatomical regions are typically the first to come into contact with the scalding bath water. In contrast, Saaiq M. et al. reported in their series that the face/head and neck were affected in 10 cases, followed by lower limbs and feet (4 cases), upper limbs and hands (3 cases), shoulder/back (2 cases), and anterior thorax and abdomen (1 case) [11].
Within the first 24 hours following estimation of the initial burned surface area, a rehydration protocol was initiated in collaboration with intensive care specialists. Third-generation cephalosporins were the most frequently administered antibiotics. Blood transfusions were performed when indicated. Burned children are particularly susceptible to hypothermia, which should be prevented through the administration of warmed fluids and the use of heated blankets [18]. In our context, treatment consisted of antiseptic bathing and application of a non-occlusive dressing with 2% aqueous eosin. Some authors have advocated for the use of occlusive dressings [19]. When burns are extensive, dressing changes under general anesthesia in the operating room are required [20].
Hospital mortality was 4.5% (1 out of 22 cases), a rate lower than those reported by other authors [7,8,11]. A favorable outcome was observed in 86.4% of cases.
CONCLUSION
Thermal burns during the neonatal period are regularly encountered in our clinical practice. The most common cause is exposure to hot liquids during bathing. As these causes are largely preventable, it is essential to educate parents of newborns to use lukewarm water when bathing their infants. Before arriving at a care facility, parents should practice cooling the burned areas with cold water.
ACKNOWLEDGEMENTS
None.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
REFERENCES
- Wassermann D. (1989). Brûlures : Etiologie, physiopathologie, diagnostic, évolution et pronostic, principes du traitement. Rev Prat. 39(30):2725-2730.
- Koç Z, Sa?lam Z. (2012). Burn epidemiology and cost of medication in paediatric burn patients. Burns. 38(6):813-819.
- Albertyn R, Bickler SW, Rode H. (2006). Paediatric burn injuries in Sub Saharan Africa--an overview. Burns. 32(5):605-612.
- Merrell SW, Saffle JR, Sullivan JJ, Navar PD, Kravitz M, Warden GD. (1986). Fluid resuscitation in thermally injured children. Am J Surg. 152(6):664-669.
- Le Touze A, Robert M, Lardy H. (2012). The management of burns in the emergency department. In: Jouve JL, Mure PY, (Edrs). Urgences chirurgicales de l'enfant. France: Wolters Kluwer. pp. 391-398.
- Ugburo AO, Fadeyibi IO, Mofikoya BO, Akanmu ON, Temiye EO, Kanu OO, et al. (2013). Neonatal burns in Lagos, South-Western Nigeria: Epidemiology and outcome of management. Burns. 39(3):483-492.
- Soudre FM, Kiba A, Kouraogo A, Karfo R, Tiendrebeogo S, Kyetega A, et al. (2021). Profil de l'ionogramme sanguine chez les enfants brûlés au CHU pédiatrique Charles De gaulles de Ouagadougou (Burkina Faso). Int J Biol Chem Sci. 15(2):426-436.
- Saaiq M, Ahmad S, Zaib S. (2013). Neonatal burn injuries: an agony for the newborn as well as the burn care team. Ann Burns Fire Disasters. 26(4):175-181.
- Amengle AL, Bengono Bengono R, Metogo Mbengono J, Beyiha G, Ze Minkande J, Obama Abena MT. (2015). Epidemiological and prognostic aspects of severe burns in children. Health Sci Dis. Vol 16 (1) January - February - March 2015. Available at: www.hsd-fmsb.org
- Zahid A, Atannaz J, Alaoui M, Rafik A, Ezzoubi M, Diouri M, et al. (2011). Profil epidemiologique des brulures d'enfants admis au Centre National des Brules, Maroc [Epidemiological profile of children burns admitted at the National Center for Brules, Morocco]. Ann Burns Fire Disasters. 24(4):171-174.
- Reynolds PR, Banerjee S, Meek JH. (2005). Alcohol burns in extremely low birthweight infants: still occurring. Arch Dis Child Fetal Neonatal Ed. 90(1):F10.
- Al-Ahdab M, Al-Omawi M. (2011). Deep partial scald burn in a neonate: a case report of the first documented domestic neonatal burn. J Burn Care Res. 32(1):e1-e6.
- Iqbal T, Saaiq M. (2011). The burnt child: an epidemiological profile and outcome. J Coll Physicians Surg Pak. 21(11):691-694.
- Golubovic Z, Parabucki D, Janjic G, Zamaklar CL, Najdanovic Z, Rakic I. (2000). The complications of burns in the newborn periods. Ann burns fire Disasters. 20(2).
- Bringué Espuny X, Soria X, Solé E, Garcia J, Marco JJ, Ortega J, et al. (2010). Chlorhexidine-methanol burns in two extreme preterm newborns. Pediatr Dermatol. 27(6):676-678.
- Ategbo S, Minto'o S, Koko J, Mengue Mba-Meyo S. (2012). Aspects épidémiologiques des accidents domestiques de l'enfant à Libreville (Gabon). Clinics in Mother and Child Health. 9(2012):C120201.
- Cox SG, Rode H, Darani AN, Fitzpatrick-Swallow VL. (2011). Thermal injury within the first 4 months of life. Burns. 37(5):828-834.
- Rimdeika R, Bagdonas R. (2005). Major full thickness skin burn injuries in premature neonate twins. Burns. 31(1):76-84.
- Sheridan RL. (2002). Burns. Crit Care Med. 30(11 Suppl):S500-S514.
- Tchaou BA, T N'venonfon CF, Houndjé Cocou YP, Avossèvou CA. (2019). Prise en Charge des Brûlures Graves de l'enfant en Réanimation à l'hôpital Universitaire de Parakou au Bénin. ESJ. 15(3):199.
 Abstract
Abstract  PDF
PDF