Past Issues
Obstructive Infracardiac TAPVR with Atypical Presentation
Jyothirmai Mallela1, Ravikumar Tenali2, Christina Karthaka3,*
1Paediatrics, Fellow Neonatology, Ravi Children's Hospital, Nellore, India
2HOD and Professor, Department of Neonatalogy and Paediatrics, Ravi Children's Hospital, Nellore, India
3Assistant Professor, Malla Reddy Medical College for Women, India
*Corresponding author: Dr. Christina Karthaka, Assistant Professor, Malla Reddy Medical College for Women, India, Phone: 9880788767, E-mail: [email protected]
Received Date: March 13, 2025
Published Date: June 13, 2025
Citation: Mallela J, et al. (2025). Obstructive Infracardiac TAPVR with Atypical Presentation. Neonatal. 6(1):24.
Copyrights: Mallela J, et al. © (2025).
ABSTRACT
Back Ground: Anamalous pulmonary venous return is one of the cardiac cause of respiratory distress in newborn and infants which is very rare and can present as early as few hours of birth till few months of age depending on type and degree of venous obstruction. It is one of the important congenital heart disease with varied clinical presentation. Newborn with obstructive TAPVR usually requires urgent intervention regardless of degree of obstruction. Surgical intervention may range from only relieving of obstruction by stenting or surgical procedure till repair and restoration of anatomical continuity between pulmonary veins and left atrium. Infracardiac TAPVC can drain into IVC or hepatic vein which is easy to access for surgery or it can drain into portal venous system which is difficult for the access. Case Presentation: A 2kg preterm (33 weeks) newborn presented to us with respiratory distress, hypoxia without cyanosis at 6 hours of life. Unsteroided mother with chest xray showed reticular shadowing. Echocardiography showed obstructed TAPVC draining into IVC.CT angiography demonstrated infracardiac TAPVC with a vertical vein going downward with an infradiaphragmatic path and stenotic lowest segment of it draining into IVC. Baby underwent an uneventful surgical repair. Conclusion: Present case highlights that diagnosis of TAPVR can be delayed or missed depending on severity of obstruction and high index of suspicion is always necessary. Also it adds that CT angiography helps in delineating cardiovascular anatomy and helps in performing palliative endovascular procedure in emergency basis where restoration of anatomical continuity between pulmonary veins and left atrium is not possible immediately.
Keywords: Anomalous Pulmonary Venous, Echocardiography, Pathophysiology, Lungs
INTRODUCTION
Total anomalous pulmonary venous connection is a rare developmental cardiac anamoly representing 1-2% [1]. It can present as an isolated defect or it could be associated with syndromes such as asplenia syndrome, holt oram syndrome, cat eye syndrome [1,2]. In TAPVR all pulmonary veins drain into systemic veins or a chamber which in turn drains into right atrium directly or indirectly bypassing right atrium [1]. Usually the obligate mixing of pulmonary and systemic venous blood will result in cyanosis in majority of cases [1,3]. Anatomical classification of TAPVR which is commonly used based on site of connection between pulmonary and systemic veins includes Supracardiac (Type 1, with anamolous connection at supracardiac level, more common), Cardiac (Type 2, with anamolous connection to coronary sinus), Infracardiac (Type 3, with anamolous connection below diaphragm) and mixed (Type 4, with mixed types of connections, which is least common type) [4]. For the fetus to survive, interatrial communication like patent foramen ovale or atrial septal defect is necessary and it is part of malformation [3]. Pulmonary edema can be seen on Chest xray due to heart failure and excessive pulmonary blood flow [1]. Obstruction to pulmonary venous blood flow is seen more commonly in infracardiac TAPVC [1]. Many reasons can be there for this, like intrinsic narrowing of connecting vessel, interposition of hepatic sinusoids between pulmonary vascular drainage and heart for those that drain via portal vein and constriction of ductus venosus [3]. This is a case report of newborn whose initial presentation is tachypnea only within few hours of life.
CASE REPORT
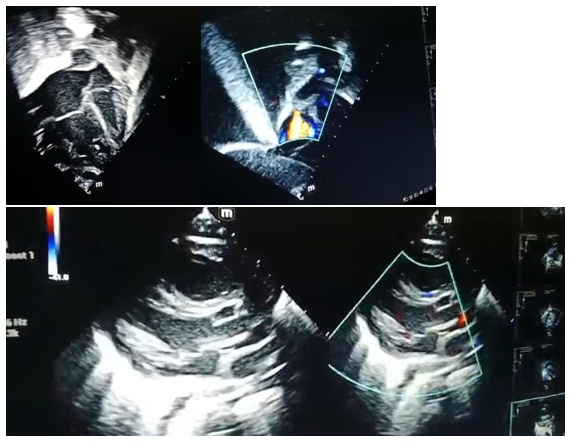
A female baby born at 33 weeks with birth weight of 2kg, born to a primi, consanguineous couple by normal vaginal delivery with APGAR scores 8? and 91? to a mother with gestational diabetes milletus. At birth baby cried immediately, Temperature of 36.5 C, HR-127/min and RR- 57/min which were normal. She was shifted to mother side and started on breast feeding. There was no family history of CHD. At 4 hours of life, baby presented to us with fast breathing and hypoxia from a local hospital. She was afebrile with respiratory rate of 72/min, HR-165/min, saturation of 80-82% in room air initially. She was initially considered to have respiratory distress syndrome and started on bubble CPAP and later on hiked up to mechanical ventilation gradually as the baby was not maintaining saturations well and persistent tachypnea was present. On mechanical ventilation with 100% Fio2, baby was maintaining saturations around 88-90%. Blood gas showed hypoxia and respiratory alkalosis. Her investigations for infection and repiratory panel were negative. Chest x-ray showed reticular shadowing. Cardiovascular examination showed normal peripheral pulses with normal heart sounds and audible murmur. Echocardiography was done to rule out cardiac causes which showed Obstructive infracardiac TAPVC. Multiple views need to be checked before getting an accurate diagnosis of CHD [5]. Subcostal imaging is important to visualize the atrial septum and to determine the direction of shunting using colour doppler [5]. Apical, left parasternal, suprasternal views are also checked along with other standard and nonstandard echocardiography views to study cardiac anatomy [5]. Suprasternal and subcostal views views need to be checked carefully to trace ascending and descending veins respectively [5]. Colour doppler and echocardiography were simultaneously done to identify direction of blood flow and anatomy respectively. As per echocardiography our case had atrial septal defect with right to left shunt. pulmonary venous drainage into left atrium is absent, instead pulmonary venous common chamber seen behind left atrium. Right side of heart is enlarged compared with left side. There is tricuspid regurgitation along with pulmonary regurgitation along with severe PAH. A large vessel was noted with venous flow draining into IVC and finally into right atrium, likely vertical vein/descending vein seen in Subcostal view. Dilated IVC drainage into right atrium and dilated pulmonary artery is observed. Vertical vein going downward with infradiaphragmatic path and stenotic lowest segment of it draining into IVC is seen in subcostal view. Echo findings supported an obstructed infracardiac TAPVC.
Case was discussed with cardiologists and was transferred to local cardiac center. Infant underwent an uneventful surgical repair of TAPVC, relieving obstruction and patch closure of secundum ASD. She has been thriving well. 5 months follow up showed unobstructed pulmonary venous flow with no acceleration, no residual communication and good biventricular systolic function.
DISCUSSION
Infracardiac TAPVC is rare form of CHD in which all pulmonary veins that bypass left atrium connect to systemic veins, right atrium or coronary sinus [1].
TAPVC accounts for 1-2% of all CHDs [1]. There is marked male preponderance for infracardiac type [1]. Echo is usually diagnostic and can identify the subtypes. cardiac catheterization is rarely performed for diagnostic purpose, it is ocassionally done to perform atrial septostomy to improve atrial shunt or identify complex mixed type of pulmonary venous return [3]. Alternatively, MRI or Cardiac CT can be used for diagnosis in complex mixed type [6].
Among cases majority are supracardiac (43%) followed by Cardiac (27%) and infracardiac (19%) and Mixed (11%) [7]. Symptoms are usually respiratory distress, cyanosis, failure to thrive and circulatory collapse, murmur and supraventricular tachycardia [8].
In obstructed infracardiac TAPVC connection is below diaphragm via long vessel which arises from common chamber in some cases [4]. Common vein descends anterior to oesophagus and then joins IVC, hepatic or portal venous system [4]. Pulmonary veinous obstruction in back pressure through pulmonary circulation resulting in Right to left shunt through an often associated ASD. Resultant pressure on Right side of heart can result in tricuspid regurgitation, enlarged main pulmonary artery together. Back pressure in lungs causes pulmonary edema. Right to left shunt results in cyanosis. Cardiac output is markedly reduced.
Pathophysiology and clinical presentation vary depending on presence of pulmonary venous obstruction(PVO), frequently seen in 75% of the cases of infracardiac TAPVC [3]. Severe PVO presents with cyanosis, respiratory failure and shock [3]. In absence of PVO, infants may present with failure to thrive, tachypnea or mild hypoxia [3].
CONCLUSION
TAPVR diagnosis in prenatal period can be challenging, but it has been associated with improved postoperative clinical status and reduced length of hospital stay. The outcome in these patients is invariably poor if not diagnosed early, for this reason high index of suspicion is always required when infant is presenting with hypoxia and tachypnea with or without cyanosis. cardiac cause should not be excluded based on normal sized heart.
ACKNOWLEDGEMENTS
None.
CONFLICTS OF INTEREST
The authors declare that there is no conflict of interest.
REFERENCES
- Park MK. (2021). Pediatric Cardiology for Practitioners. 7th Edition, Mosby Elsevier, Philadelphia. pp. 186-189.
- Lim WK, Wong MN, Tan SK. (2014). Emergency stenting of vertical vein in a neonate with obstructed supracardiac total anomalous pulmonary venous drainage. Med J Malaysia. 69(3):138-139.
- Al-Mutairi M, Aselan A, Al-Muhaya M, Abo-Haded H. (2020). Obstructed infracardiac total anomalous pulmonary venous connection: The challenge of palliative stenting for the stenotic vertical vein. Pediatr Investig. 4(2):141-144.
- Pereira SS, Meinerikandathevan S. (2022). Infracardiac Total Anomalous Pulmonary Venous Drainage: A Case Report. Journal of Diagnostic Medical Sonography. 38(5):452-456.
- Siassi B, Noori S, Acherman RJ, Wong PC. (2019). Practical Neonatal Echocardiography. China: McGraw-Hill Publication.
- Chowdhury UK, Airan B, Malhotra A, Bisoi AK, Saxena A, Kothari SS, et al. (2008). Mixed total anomalous pulmonary venous connection: anatomic variations, surgical approach, techniques, and results. J Thorac Cardiovasc Surg. 135(1):106-116.
- Seale AN, Uemura H, Webber SA, Partridge J, Roughton M, Ho SY, et al. (2010). Total anomalous pulmonary venous connection: morphology and outcome from an international population-based study. Circulation. 122(25):2718-2726.
- Lemaire A, DiFilippo S, Parienti JJ, Metton O, Mitchell J, Hénaine R, et al. (2017). Total Anomalous Pulmonary Venous Connection: A 40 years' Experience Analysis. Thorac Cardiovasc Surg. 65(1):9-17.
 Abstract
Abstract  PDF
PDF