Current Issue
Congenital Heart Disease in Neonates: Diagnosis and Clinical Profile in A Morrocan Intensive Care Unit
A Ayad*, S Sghir, M Sellouti, R Abilkacem
Neonatal Intensive Care Unit, Military Hospital of Rabat, Morocco
*Corresponding author: Anass Ayad, Neonatal Intensive Care Unit, Military Hospital of Rabat, Morocco, Phone: 0661315979, E-mail: [email protected]
Received Date: September 11, 2025
Published Date: October 29, 2025
Citation: Ayad A, et al. (2025). Congenital Heart Disease in Neonates: Diagnosis and Clinical Profile in A Morrocan Intensive Care Unit. Neonatal. 6(2):26.
Copyrights: Ayad A, et al. © (2025).
ABSTRACT
Background: Congenital heart disease (CHD) is the most common congenital anomaly and a major cause of neonatal morbidity and mortality. Data on neonatal CHD in Morocco remain scarce. Objective: To describe the clinical profile, risk factors, management, and outcomes of neonates with CHD admitted to a Moroccan tertiary neonatal intensive care unit (NICU). Methods: A retrospective review was conducted over a 4-year period (2020–2024). Neonates with echocardiographically confirmed CHD were included, excluding minor lesions such as patent foramen ovale or small atrial septal defect. Clinical presentation, risk factors, therapeutic modalities, and outcomes were analyzed. Results: Among 150 neonates screened, 75 were diagnosed with CHD (62% male). Consanguinity (34%) and maternal infections especially viral ones (20%) were the most frequent risk factors. The most common presenting symptoms were respiratory distress (88%) and feeding difficulties (85%). Acyanotic lesions predominated (63%), with VSD being the most frequent (26%). Among cyanotic lesions, TOF and TGA were the most common. Mortality was high, particularly in complex cyanotic CHD, while acyanotic lesions showed better short-term survival. Conclusion: CHD is a significant contributor to neonatal morbidity and mortality in Morocco. Strengthening antenatal screening, early diagnosis, and referral to pediatric cardiac centers is essential to improve outcomes.
Keywords: Congenital Heart Disease, Neonate, Cyanotic Heart Disease, Ventricular Septal Defect, Transposition of Great Arteries, Outcome, Mortality, Morocco.
INTRODUCTION
Congenital heart diseases (CHD) refers to structural or functional heart diseases at birth. These are primarily seen in neonates, infants or children, the incidence of moderate to severe structuralcongenital heart disease in live born infant is 6 to 8 per 1000 livebirths [1]. About 2-3 per 1000 newborn will be symptomatic with heart disease in 1st year of life.
Congenital heart diseases are the most prevalent and serious of all recognized structural birth defects. The burden of CHD in morocco is likely to be enormous, due to a Many cases are asymptomatic and discovered incidentally during routine health check-up. Even though there are numerous different cardiac lesions, there are many similarities in their clinical presentation. Signs and symptoms of severe heart disease in the newborn period include cyanosis, discrepant pulses and blood pressures, congestive heart failure, and cardiogenic shock.
The initial evaluation of any newborn suspected of having critical congenital heart disease includes a meticulous physical exam, four extremity blood pressures, preductal and postductal saturations, hyperoxia test, chest radiograph, ECG and echoicardiography that has become the primary diagnostic tool for CHD reducing the requirement for invasive studies such as cardiac catheterization.
There is lack of data about spectrum of CHD in neonatesin our country. The aim of the study was to describe clinical profile and available therapeutic modalities used in the management of CHD in neonatal intensive care unit (NICU) at Rabat military hospital.
MATERIEL AND METHODS
Retrospective analysis of the medical records of a 4-year period (January 2020 to December 2024) was performed in a neonatal intensive care unit (NICU) of rabat military Hospital, which is a referral medical center in morocco. The number of patients admitted to the NICU during the four -year period was A total of 150 patients underwent echocardiography for various reasons.
Excluding cases with patent ductus arteriosus (PDA) in prematurity, patent foramen ovale (PFO) and small secondum atrial septal defect (ASD) (≤3 mm), and minimal peripheral pulmonic stenosis (PS) (peak flow velocity≤2.0 m/sec), a total of 75 patients (50% of total inpatients) diagnosed with CHD was included as subjects in this study (58males and 17 females). Among these patients with CHD, 70 patients were born at our institution and 5 patients were born at local hospitals or clinics and transferred to our institution with various symptoms and signs.
Whereas most of all the inborn patients underwent antenatal echography, none were diagnosed with CHD antenatally on the fetal echocardiography, it was hard to get detailed information on the antenatal care at local primary obstetrical clinics and all of them were diagnosed with CHD postnatally.
Median age of patients at admission was 1 day after birth (ranging from the first day of life to 29 days) and median birth weight was 2,860 g (810 to 5,700 g);
Echocardiography has been performed by a single pediatric cardiologist at NICU using M-mode, Two-dimensional Color Doppler cardiac imaging, 7 MHz, 5 MHz-transducers frequency by the mean of Two-dimensional ECHO (Vivid 3). All therapeuticmodalities used in management of CHD were documented.
RESULTS
Table 1 depicts the time of presentation of new-born with congenital heart disease. Nearly half of the cases presented in the first week (52%) followed by those in third week (22%), fourth week (%), second week (7%) in decreasing order.
Table 1. Age at presentation of new born with CHD
|
AGE |
No. of cases (n) |
(%) |
|
Week 1 |
39 |
52 |
|
Week2 |
8 |
10 |
|
Week3 |
15 |
20 |
|
Week4 |
13 |
17 |
Table 2 shows the sex distribution of the neonates included in the study. 54% were male and 46% were female.
Table 2. Sex distribution of new-born with CHD
|
SEX |
No of Cases (n) |
Percentage (%) |
|
MALE |
58 |
78 |
|
FEMALE |
17 |
22 |
The commonest risk factors encountered among the studied neonates were positive parental consanguinity (40%), followed by Maternal infections (36%), especially viral ones such as Epstein–Barr virus (EBV), cytomegalovirus (CMV), rubella, parvovirus B19, or toxoplasmosis, have been associated with CHD.
These infections may lead to direct myocardial damage, endocardial fibroelastosis, or interfere with cardiac morphogenesis during the early stages of fetal development.
Among them, rubella infection in the first trimester is classically linked to patent ductus arteriosus, pulmonary stenosis, and ventricular septal defects.
THE POSSIBLE RISK FACTORS OF CCHD
|
Riskfactors |
No of cases |
Percentage (%) |
|
Consanguinity |
30 |
40 |
|
Maternal infection |
27 |
36 |
|
Family history |
15 |
20 |
|
Maternal drugs |
3 |
4 |
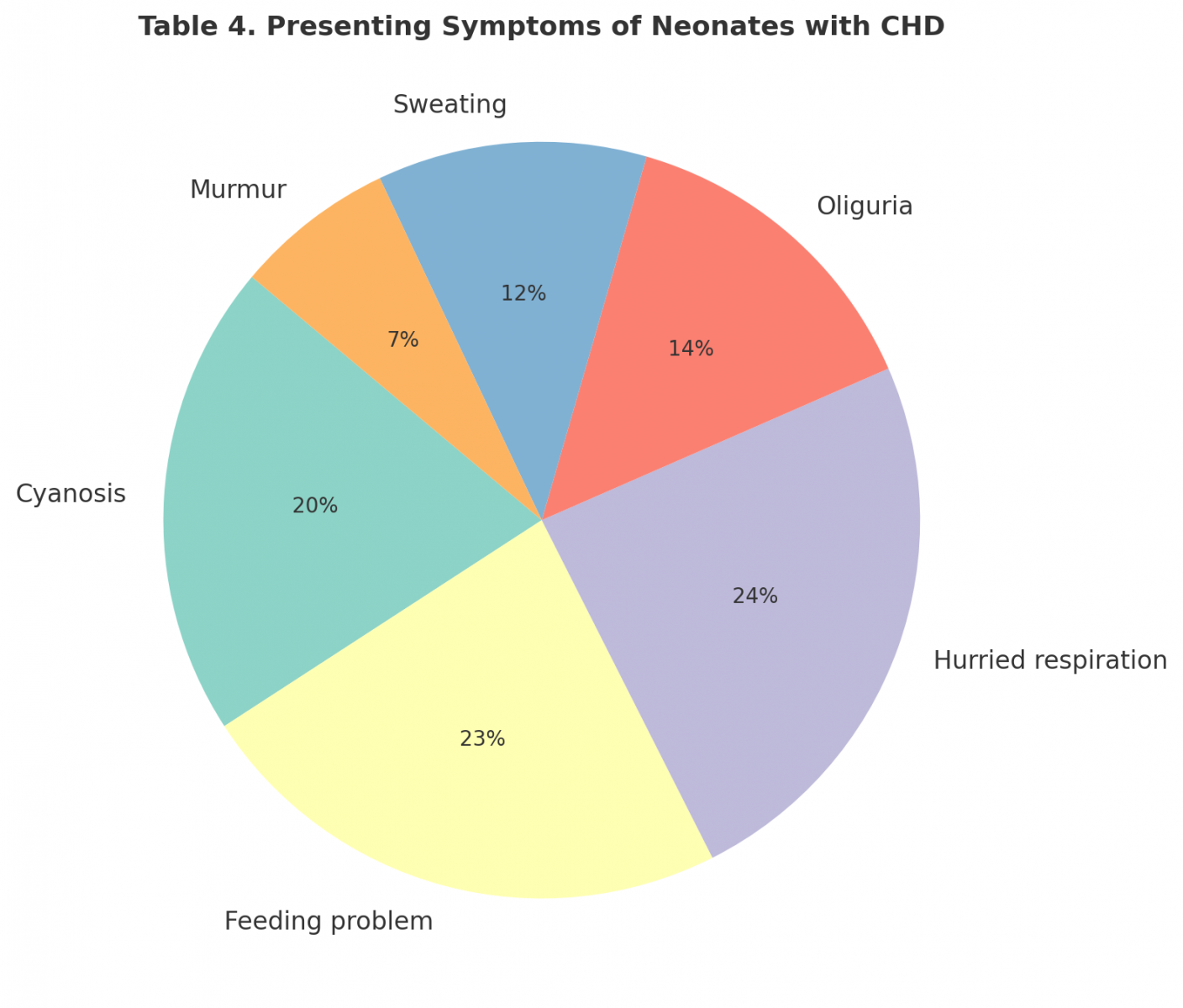
As evident from the below figure, the commonest presenting complaint was respiratory distress (88%), followed by feeding problem, cyanosis and congestive cardiac failure manifested as decreased urinary output and excessive forehead sweating. (25%) were asymptomatic and clinically only murmur was present.
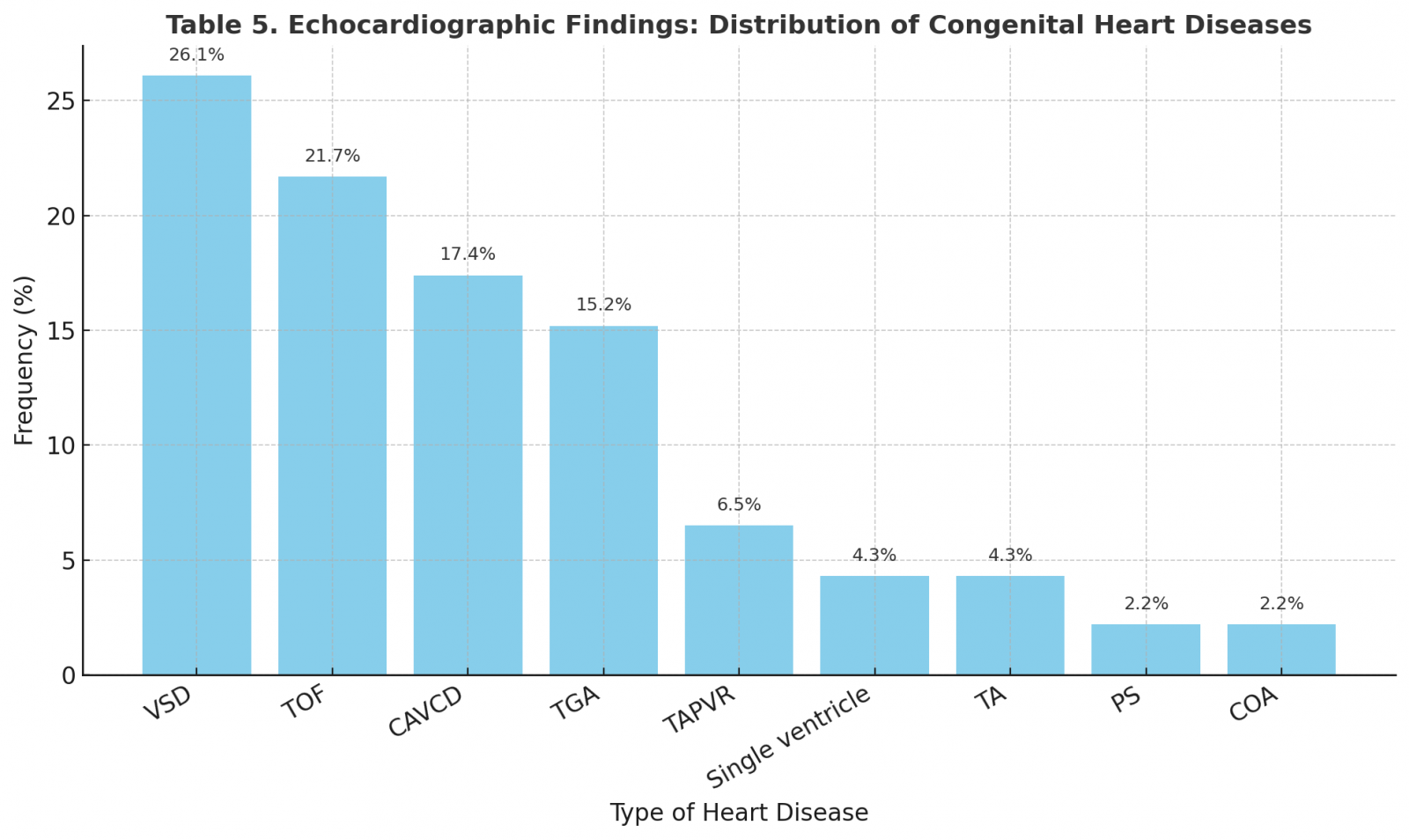
Majority of the cases (63%) were acyanotic type, remaining being cyanotic.
Among the cyanotic, tetralogy of fallot was the commonest, followed by transposition of great arteries. In the acyanotic group, ventricular septal defect was the commonest, followed by atrio-ventricular canal defect. Most of the cyanotic CHD, presented within the 1st week of life while acyanotic CHD presented in the 2th week of life (Table 5).
All cases needed medical treatment in the form of one or more of the following Prostaglandin E1 (PGE1) infusion, anti failure inotropes, antibiotics, vitamin K or sodium bicarbonate.
Balloon atrial septostomy was performed 2 cases. Seven neonates required mechanical ventilation while oxygen therapy was used in 70 patients.
In our series, neonatal mortality related to congenital heart disease (CHD) was substantial. Survival strongly depended on the type of malformation and the therapeutic modalities available. Infants with complex cyanotic lesions, such as transposition of the great arteries (TGA), or single ventricle physiology, showed the poorest outcome in the absence of timely surgical intervention. The overall mortality in our cohort is consistent with rates reported in developing countries, ranging between 25–45%. Conversely, acyanotic lesions such as isolated ventricular septal defect (VSD) or partial atrioventricular canal defects were associated with better short-term outcome, though these patients remain at risk for heart failure, recurrent infections, and growth impairment. The need for advanced support including mechanical ventilation or continuous prostaglandin infusion was strongly correlated with increased morbidity and mortality, reflecting the severity of the underlying cardiac defect.
DISCUSSION
Congenital heart disease (CHD) is the most common congenital malformation and remains a major cause of neonatal morbidity and mortality worldwide. The incidence has been consistently reported between 6 and 8 per 1,000 live births in population-based studies [2,3]. In our study, conducted in a Moroccan tertiary NICU, 75 neonates were diagnosed with significant CHD over a four-year period,
The distribution of lesions in our cohort shows that ventricular septal defect (26%) was the most frequent acyanotic lesion, followed by atrioventricular canal defect (17%). Among cyanotic malformations, tetralogy of Fallot (22%) and transposition of the great arteries (15%) predominated. This spectrum is comparable to large population-based reports where VSD represents 20–30% of all cases [4,5], and TOF and TGA are the leading cyanotic lesions [6,7]. In contrast, Egyptian and Indian NICU-based studies have reported a higher proportion of TGA and complex cyanotic lesions, reflecting referral bias in tertiary care units. Our series, with a predominance of VSD and TOF, aligns more closely with community-based distributions, though still enriched in severe forms due to NICU selection.
Consanguinity was observed in 40% of our cases, consistent with reports from other Middle Eastern and North African populations where parental consanguinity is a well-recognized risk factor. Maternal drug intake and infections in early pregnancy were also documented, echoing findings by Grech and Gatt in Malta and by Malik et al. in the U.S., where environmental and genetic factors interplay in the pathogenesis of CHD [8,9].
Most neonates presented within the first week of life, with respiratory distress, feeding problems, and cyanosis as the predominant symptoms. This is in line with previous studies noting that early manifestations are often non-specific and can mimic sepsis or primary pulmonary disease. Delayed recognition remains a challenge, particularly in the absence of antenatal detection. In our study, no cases were diagnosed prenatally, despite routine obstetric ultrasounds. This contrasts with data from Korea and France, where the introduction of systematic fetal echocardiography has markedly improved prenatal detection and influenced disease patterns and survival [10,11].
The overall outcome in our series highlights the vulnerability of neonates with complex cyanotic lesions. Mortality was disproportionately high among infants with TGA, single ventricle physiology, and CAVCD, whereas those with isolated VSD had a better short-term prognosis. These findings are consistent with the literature: neonates with duct-dependent systemic or pulmonary circulation have the worst early survival unless timely intervention is provided.
In India, Ravilala et al. reported a 42% neonatal mortality rate among CHD cases, while the Egyptian series by Abou-Taleb et al. noted a 26% in-hospital mortality, mainly in HLHS and complex malformations. Our mortality rates fall within this range, reflecting similar challenges of limited access to pediatric cardiac surgery. In contrast, studies from developed countries show significantly improved outcomes with early surgical and interventional strategies, emphasizing the role of timely referral and specialized centers [8,9].
Classic population studies such as Mitchell et al. (1971) and Hoffman (1995, 2002) established the baseline incidence of CHD at ~0.8% of live births, with VSD being the most common lesion. More recent Asian data confirm similar patterns, though regional differences exist, such as higher rates of TOF in China and Taiwan [12]. Our Moroccan data align with these global distributions but reveal a persistently high neonatal mortality, more comparable to reports from other low- and middle-income settings. The absence of prenatal diagnosis in our cohort contrasts with trends in Korea, France, and the U.S., where fetal echocardiography has significantly reduced perinatal mortality by enabling planned deliveries in tertiary centers [13].
CONCLUSION
Congenital heart diseases represent a major cause of neonatal morbidity and mortality in Morocco. Acyanotic lesions, particularly VSD, were the most common, while TGA and TOF dominated the cyanotic group. Outcome was strongly influenced by the type of malformation, availability of intensive care support, and access to surgical correction. Improving antenatal diagnosis, enhancing neonatal screening, and establishing timely referral pathways to specialized cardiac centers are crucial steps to improve survival.
ACKNOWLEDGEMENTS
None.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest related to this study.
FUNDING
No funding was received for the conduct of this study or the preparation of this manuscript.
REFERENCES
- Mitchell SC, Korones SB, Berendes HW. (1971). Congenital heart disease in 56,109 births. Incidence and natural history. Circulation. 43(3):323-332.
- Grech V, Gatt M. (1999). Syndromes and malformations associated with congenital heart disease in a population-based study. Int J Cardiol. 68(2):151-156.
- Jung SC, Kim SS, Yoon KS, Lee JS. (1999). Prevalence of congenital malformations and genetic diseases in Korea. J Hum Genet. 44(1):30-34.
- Hoffman JI. (1995). Incidence of congenital heart disease: I. Postnatal incidence. Pediatr Cardiol. 16(3):103-113.
- Kovalchin JP, Silverman NH. (2004). The impact of fetal echocardiography. Pediatr Cardiol. 25(3):299-306.
- Chung ML, Lee BS, Kim EA, Kim KS, Pi SY, Oh YM, et al. (2010). Impact of fetal echocardiography on trends in disease patterns and outcomes of congenital heart disease in a neonatal intensive care unit. Neonatology. 98(1):41-46.
- Levey A, Glickstein JS, Kleinman CS, Levasseur SM, Chen J, Gersony WM, et al. (2010). The impact of prenatal diagnosis of complex congenital heart disease on neonatal outcomes. Pediatr Cardiol. 31(5):587-597.
- Geggel RL. (2004). Conditions leading to pediatric cardiology consultation in a tertiary academic hospital. Pediatrics. 114(4):e409-e417.
- Jung JW, Kim NS, Lee SY, Park IS. (2010). Recent trends in the frequency of congenital heart diseases: nationwide survey in Korea. Abstract, 3rd Congress of Asia-Pacific Pediatric Cardiac Society; Chiba, Japan. pp. 225.
- Hoffman JI, Kaplan S. (2002). The incidence of congenital heart disease. J Am Coll Cardiol. 39(12):1890-1900.
- Lee JE, Jung KL, Kim SE, Nam SH, Choi SJ, Oh SY, et al. (2010). Prenatal diagnosis of congenital heart disease: trends in pregnancy termination rate, and perinatal and 1-year infant mortalities in Korea between 1994 and 2005. J Obstet Gynaecol Res. 36(3):474-478.
- Wu MH, Chen HC, Lu CW, Wang JK, Huang SC, Huang SK. (2010). Prevalence of congenital heart disease at live birth in Taiwan. J Pediatr. 156(5):782-785.
- Yang XY, Li XF, Lü XD, Liu YL. (2009). Incidence of congenital heart disease in Beijing, China. Chin Med J (Engl). 122(10):1128-1132.
 Abstract
Abstract  PDF
PDF