Past Issues
Symptomatic Congenital Lung Lesions in Premature Newborns: Do Less to Do Better. A Cases Series
Sara Silvaroli*, Filomena Valentina Paradiso, Riccardo Rizzo, MariaVittoria Stern, Lorenzo Nanni
Unit of Paediatric Surgery, Department of Woman and Child Health and Public Health, Fondazione Policlinico Universitario A. Gemelli IRCCS, Rome, Italy
*Corresponding author: Sara Silvaroli, Unit of Paediatric Surgery, Department of Woman and Child Health and Public Health, Fondazione Policlinico Universitario A. Gemelli IRCCS, Rome, Italy; Email: [email protected]
Received Date: January 31, 2024
Publication Date: March 18, 2024
Citation: Silvaroli S, et al. (2024). Symptomatic Congenital Lung Lesions in Premature Newborns: Do Less to Do Better. A Cases Series. Neonatal. 4(1):14.
Copyright: Silvaroli S, et al. © (2024).
ABSTRACT
Congenital lung lesions (CLL) refer to different histopathologies. The most common types are congenital cystic adenomatoid malformations (CCAM) and bronchopulmonary sequestrations (BPS) or hybrid lesions containing features of both. Congenital lobar emphysema (CLE) and bronchogenic cysts (BC) are less common. Different opinions exist on treatment of CLL in symptomatic neonates. Though immediate surgery appears a reasonable option, the risks related to neonatal surgery should be balanced with those of conservative treatment. We analyzed complications and outcomes of four symptomatic neonates diagnosed with CLL presenting with severe symptoms at birth: two underwent emergency surgery and two underwent a conservative management in the neonatal period. A better outcome was observed in those who avoided surgery at birth. Emergency surgery in symptomatic neonates should be always evaluated, if possible avoided, with other strategies like chest drain, ventilation, inotrope support. Furthermore, we stress the need for more scientific evidence and guidelines supporting surgeons making the right decision.
Keywords: Congenital lung malformation; Neonatal surgery; Neonatal respiratory distress; CCAM; Premature ventilation
INTRODUCTION
Congenital lung lesions are rare congenital anomalies with an estimated incidence of one in every 25,000 to 35,000 births [1-9]. These congenital parenchymal lung diseases are characterized by the over-proliferation and dilatation of terminal bronchioles with the absence of normal alveoli [10]. CLL comprise a heterogeneous group of histologic types often diagnosed during prenatal ultrasound screening at 18-20 weeks of gestation [11]. Their general prenatal course is well described, particularly concerning larger lesions. Fetal clinical presentation varies: most lesion peak in size around 28-30 weeks of gestation and potentially regress at the end of pregnancy in 43%-86% of neonates resulting in an asymptomatic birth [3,11].
In a small percentage of cases, extensive lesions, often correlate to congenital pulmonary airway malformation volume-ratio (CVR) > 1.6 (2), are associated to severe hydropes, fetal edema and severe ascites with or without mediastinal shift and subsequent fetal heart failure [2,12]. Possible fetal procedures include minimally invasive thoracoamniotic shunt placement, open fetal resection of large and severe symptomatic lesions [13], or delivery by ex-utero intrapartum treatment (EXIT) with resection of the lesion [12].
CASES DESCRIPTION
Case 1
Female (2500g) born preterm (34 GW).
An amnioreduction and two in utero left thoracentesis were performed because of polyhydramnios, mediastinal shift and a left hydrothorax.
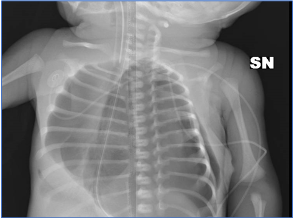
The newborn presented at birth with respiratory distress and pulmonary hypertension requiring ventilation and nitric oxide. Left thoracentesis and chest drainage for a hypertensive pneumothorax (Figure 1) were performed. A partial abnormal pulmonary venous return was diagnosed after birth by cardiac ultrasound.
Figure 1: Case 1 RX: Massive pneumothorax with acute respiratory distress.
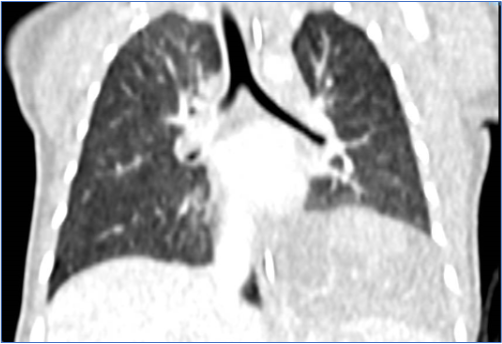
Oscillatory ventilation was maintained for 120 hours and the chest tube was removed on day eight. CT scan confirmed an extralobar sequestration, 4 x 4 cm, supplied by two arteries, which were connected with the thoracic aorta (Figure 2). The neonate was discharged at day 18 and was followed up cardiologically for four months until thoracoscopic surgery. She was discharged after three days, because of an uneventful post-operative period. At 12 months follow-up, no complications were observed.
Figure 2: Case 1 CT: extralobar sequestration 4 x 4 cm large supplied by two arteries, connected with the thoracic aorta.
Case 2
Male (1700g) born preterm (31 GW)
Prenatal ultrasound was unremarkable. At birth, bronchopulmonary dysplasia and left pneumothorax were treated with non-invasive ventilation and surfactant. After five days the newborn’s respiratory parameters normalized and ventilator support was terminated.
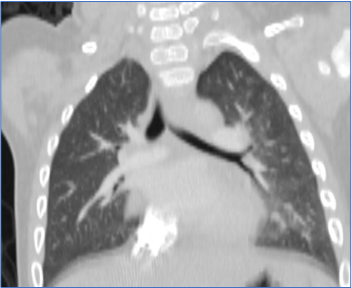
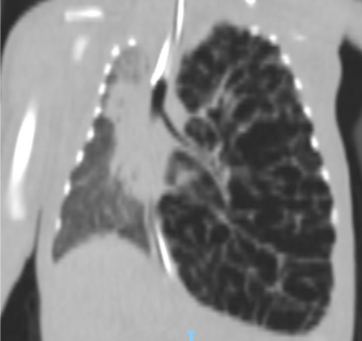
After two weeks, following an episode of new respiratory distress, chest x-ray showed a left pneumothorax with mediastinal shift; a congenital diaphragmatic hernia was suspected. Chest CT-scan depicted a CCAM, involving the entire left lung (Figure 3). Additionally, a mediastinal shift, right lower lobe consolidation and localized anterior pneumothorax were documented. The bronchoalveolar lavage was positive for Enterococcus faecium and Klebsiella Pneumoniae.
Figure 3: Case 2 CT: CCAM involving the entire left lung with mediastinal shift, right lower lobe consolidation and localized anterior pneumothorax.
In a multidisciplinary meeting, lung infection was deemed a contraindication for any surgical approach; moreover, malformation extent would have requested a pneumonectomy. Therefore, a conservative treatment was decided including oscillatory ventilation, CT scan guided chest drainage and antibiotic therapy. Unexpectedly, the neonate pneumothorax spontaneously improved and no invasive procedures were needed. The baby was extubated after 15 days and discharged after three weeks. Clinical follow-up with CT-scan after 6 months showed neither cystic lesions, pneumothorax nor abnormal pulmonary parenchyma (Figure 4) At 12 months follow up, no complications were observed.
Figure 4: Case 2 second CT: after 6-month absence of cystic lesions, pneumothorax or abnormal pulmonary parenchyma.
Case 3
Male (1100g) born preterm (27 GW).
Prenatal screening was unremarkable. At birth, a bronchopulmonary dysplasia and pulmonary hypertension were treated with oscillatory ventilation, surfactant and nitric oxide. At day four, a chest x-ray revealed a right pneumothorax, which was treated with chest drainage for four days.
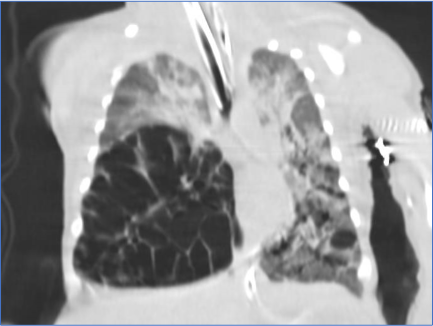
A respiratory distress episode occurred on day 12. A chest x-ray followed by a CT-scan showed a right pneumothorax, mediastinal shift, emphysema of middle and lower right lobes and bilateral upper lobe consolidation (Figure 5-6).
Figure 5: Case 3 RX: right pneumothorax with mediastinal shift.
Figure 6: Case 3 CT: emphysema of middle and lower right lobes and bilateral upper lobe consolidation.
An emergency right thoracotomy and middle and lower lobectomies were performed. After surgery, the chest tube was maintained for 10 days and mechanical ventilation for 27 days. The baby was discharged after three months.
At three years follow-up, the child is doing well showing normal growth.
Case 4
Male (780g) born preterm (25 GW) with normal prenatal ultrasound findings
At birth, a bronchopulmonary dysplasia and pulmonary hypertension were treated with oscillatory ventilation, surfactant, nitric oxide and sildenafil. Two episodes of pulmonary bleeding and mycotic pneumonia required treatment.
During the first two weeks, serial chest x-rays were performed as follow up on a chest infection until day 18 when a CT-scan revealed left lung emphysema with mediastinal shift and lower and middle right lobe consolidations (Figure 7). The neonate’s critical condition, without possibility to ventilate, required an emergency left pneumonectomy.
Figure 7: Case 4 CT: left lung emphysema with mediastinal shift and lower and middle right lobe consolidation.
His general condition gradually deteriorated. The child died three days after surgery, despite oscillatory ventilation with maximal parameters, nitric oxide together with sildenafil and inotropic therapy.
DISCUSSION
We analyzed characteristics and outcomes of four symptomatic preterm neonates affected by different CLL forms (Table 1) CLE (two), bilobar CCAM (one), and BPS (one). One of these malformations was diagnosed and treated prenatally by thoracentesis and amnioreduction. Unfortunately, we have no information about our patients’ CVR because they were all prenatally diagnosed in other centers. All our patients presented with symptoms at birth or in the first days of life. Two neonates affected by emphysema, underwent emergency surgery; one, underwent lobectomy and survived; the other, underwent pneumonectomy and died.
|
|
Case 1 |
Case 2 |
Case 3 |
Case 4 |
|
GESTATIONAL WEEKS |
34 + 4 |
31 + 2 |
27 + 4 |
25 + 2 |
|
BIRTH WEIGHT |
2500 g |
1710 g |
1100 g |
780 g |
|
PRENATAL SIGNS A: Hydrothorax B: Mediastinal shift C: Polyhydramnios D: Ascites |
A + B+ C |
None |
None |
None |
|
PRENATAL TREATMENT A: Amnioreduction B: Thoracentesis |
A: 1 time, B: 2 times |
None |
None |
None |
|
RADIOLOGY Prenatal Postnatal |
MRI CT scan |
Ultrasound CT scan |
Ultrasound CT scan |
Ultrasound CT scan |
|
BIRTH CONDITIONS |
Distress |
Distress, HMD |
Asymptomatic |
Distress, HMD, PH |
|
HEART MALFORMATION |
TAPVR + ASD + PFO |
PFO |
PDA, MH |
PDA, MH |
|
CLL TYPE |
extralobar BPS |
left lung CCAM |
Bilobar CLE |
Lobar CLE |
|
SURGICAL INTERVENTION (D: day after birth) |
D1: chest tube 4 months: thoracoscopic resection |
No |
D12: Bilobectomy |
D15: Pneumectomy |
|
COMPLICATIONS |
None |
None |
None |
Respiratory failure |
|
PROGNOSIS |
Alive |
Alive without intervention |
Alive |
Died |
|
FOLLOW-UP |
Asymptomatic |
Asymptomatic |
Asymptomatic |
None |
Table 1: Results; Results Abbreviations: PDA: patent Ductus Arteriosus; ASD: Atrial Septal Defect; PFO: Patent Foramen Oval; TAPVR: Total Anomalous Pulmonary Venous Return; CCAM: Congenital Cystic Airways Malformation; CLE: Congenital Lobar Emphysema; BPS: Broncho Pulmonary Sequestration; HMD: Hyaline Membrane Disease; MH: Myocardial Hypertrophy; PH: Pulmonary Hypertension; MD: Myocardial Dyskinesia.
The remaining two neonates were non-surgically managed in emergency. In one of the neonates chest drainage at birth was performed and lobectomy at four months of age and the other pulmonary malformation spontaneously resolved. Both children are alive without respiratory symptoms or sequelae and have been followed up for at least one year.
Postnatal CLL management is still debated. There are four arguments used to justify a surgical approach to manage asymptomatic CLL: the risk of malignancy, the risk of complications including infection and pneumothorax, the potential for compensatory lung regrowth following early resection and reduction in postoperative complications following elective surgery [14]. Although CLL was generally considered a benign lesion, several studies reported increased risk of malignancy in patients with CLL; however, the relationship between CLL and malignancy remained unclear [13]. Moreover, in several studies, bronchioloalveolar carcinoma and pulmonary rhabdomyosarcoma has been reported in association with CLL [15-17]. Other authors consider that prophylactic resection of cystic lung lesions does not eliminate the risk of malignancy. For example, adenocarcinoma has been described following a previous resection of congenital pulmonary airway malformation in early life and a pleuropulmonary blastoma was described following prior resection of a cystic lesion from an anatomically distinct area of the lung [18]. Concerning the outcome of patients treated for symptomatic CLL, some authors suggest that those patients experience a longer and more complicated postoperative clinical course, underwent longer mechanical ventilation, pleural drainage, and hospitalization [19]. Other authors recommend surgery only after infection or symptom development [7,8].
The indication for elective surgery, based on the possibility that alveolar regeneration was thought to be more likely in early life during the alveolar stage of lung growth, was contested by some authors [21,22] describing the absence of clear evidence for this phenomenon and the proof for new alveolar growth in adolescence [23].
However, surgical management in symptomatic neonates at birth remains unquestioned. In the literature, few reports exist about lung resections in symptomatic newborns at birth, and even fewer reports regarding premature babies. Some authors consider neonatal pulmonary surgery, even for an emergency, as safe because of a low mortality and morbidity risk [12,20,24]. Despite this, we agree with the authors of a systematic review and meta-analysis about postnatal CLL management [4], who analyzed early and late complications of emergency versus elective surgery in symptomatic neonates and infants. The meta-analysis included 1070 patients, and authors concluded that elective surgery was associated with significantly less complications than emergency surgery in all age ranges. The risk ratio was 2.8 (95% CI, p<0.005) comparing complications after elective surgery with emergency surgery.
Even elective surgery is not without risk. In a study about asymptomatic infants, complications occurred in 5%, which included air leak, infection, effusion and death in one case [4]. Recently, in a cohort of 60 patients with asymptomatic CLL, who underwent surgery, a complication rate of 23% was reported including three major complications: tension pneumothorax, aggressive chest wall fibromatosis and near fatal haemorrhage [23].
We believe that the distinctive trait of our series is the severe manifestation at birth caused by the extension of the lesions in premature babies. In our cases, the surgical procedure was necessary as a life-saving manoeuvre, after applying alternative therapeutic possibilities (ventilation, inotropes, and nitric oxide). We are aware of three possible biases in our series: the first is prematurity, the second is cardiological comorbidity in all cases and the third is the extension of the malformation, which in two cases included the entire lung. We are aware that from our case series, presenting four cases, no final conclusion can be drawn. However, analyzing our clinical records and available literature, we would like to stress that emergency surgery should be the last treatment option in neonates for its impact on quality of life and not be seen as standard of care.
CONCLUSION
In conclusion, because of poor survival prognosis and impact on quality of life, we recommend favouring always first other strategies like chest drain, ventilation, inotrope support. This is more important for the premature neonate and if the malformation is extensive. We would like to stress the need for further multicentric studies to develop guidelines, which could support the surgeon and the paediatric multidisciplinary team in its decision process.
REFERENCES
- Cass DL, Crombleholme TM, Howell LJ, Stafford PW, Ruchelli ED, Adzick NS. (1997). Cystic lung lesions with systemic arterial blood supply: a hybrid of congenital cystic adenomatoid malformation and bronchopulmonary sequestration. J Pediatr Surg. 32:986-990.
- Crombleholme TM, Coleman B, Hedrick H, Liechty K, Howell L, Flake AW, et al. (2002). Cystic adenomatoid malformation volume ratio predicts outcome in prenatally diag nosed cystic adenomatoid malformation of the lung. J Pediatr Surg. 37:331-338.
- Davenport M, Warne SA, Cacciaguerra S, Patel S, Greenough A, Nicolaides K. (2004). Current outcome of antenatally diagnosed cystic lung disease. J pediatr Surg. 39:549-556.
- Stanton M, Njere I, Ade-ajayi N, Patel S, Davenport M. (2009). Systematic review and meta-analysis of the post-natal management of congenital cystic lung lesions. J Pediatr Surg. 44:1027-1033.
- Parikh D, Samuel M. (2005). Congenital cystic lung lesions: is surgical resection essential. Pediatr Pulmonol 40:533-537.
- Jarrett M, Hanmin L, Lan V. (2017). Thoracoscopic lobectomy for congenital lung lesions. Clin Perinatol. 44:781-794.
- Aziz D, Langer JC, Tuuha SE, Ryan G, Ein S H, Kim PC. (2004). Perinatally diagnosed asymptomatic congenital cystic adenomatoid malformation: to resct or not. J pediatr Surg. 39:329-334.
- Chetcuti PS, Crabbe DC. (2006). CAM lungs: the conservative approach. Arch Dis Child Fetal Neonatal Ed. 91:463-464.
- Laberge JM, Puligandla P, Flageole H. (2005). Asymptomatic congenital lung malformations. Semin Pediatr Surg. 14:16-33.
- Durell J, Lakhoo K. (2014). Congenital cystic lesions of the lung. Early Hum Dev. 90:935-939.
- Kunisaki SM, Barnewolt CE, Estroff JA, Ward VL, et al. (2021). Actualizacion en medicina maternofetal. J Pediatr Surg. 42:404-410.
- Fan D, Wu S, Wang R, Huang Y, Fu Y, Ai W, et al. (2017). Successfully treated congenital cystic adenomatoid malformation by open fetal surgery A care-compliant case report of a 5-year follow-up and review of the literature. Medicine (Baltimore). 96:e5865.
- Cook J, Chitty L S, De Coppi P , Ashworth M , Wallis C. (2017). The natural history of prenatally diagnosed congenital cystic lung lesions: long-term follow-up of 119 cases. Arch Dis Child. 102:798-803.
- Sudou M, Sugi K, Murakami T. (2003). Bronchioloalveolar carcinoma arising from a congenital cystic adenomatoid malformation in an adolescent: The first case report from the Orient. J Thorac Cardiovasc Surg. 126:902-903.
- Lantuejoul S, Nicholson AG, Sartori G, Piolat C, Danel C, Brabencova E, et al. (2007). Mucinous cells in type 1 pulmonary congenital cystic adenomatoid malformation as mucinous bronchioloalveolar carcinoma precursors. Am J Surg Pathol 31:961-969.
- Federici S, Domenichelli V, Tani G, Sciutti R, Burnelli R, Dòmini R. (2001). Pleuropulmonary blastoma in congenital cystic adenomatoid malformation: report of a case. Eur J Pediatr Surg 11:196-199.
- Papagiannopoulos KA, Sheppard M, Bush AP, Goldstraw P. (2001). Pleuropulmonary blastoma: is prophylactic resection of congenital lung cysts effective? Ann Thorac Surg. 72:604-605.
- Conforti A, Aloi I, Trucchi A, Morini F, Nahom A, Inserra A, et al. (2009). Asymptomatic congenital cystic adenomatoid malformation of the lung: is it time to operate? J Thorac Cardiovasc Surg. 138:826-830.
- Shanmugam G, MacArthur K, Pollock JC. (2005). Congenital lung malformations-antenatal and postnatal evaluation and management. Eur J Cardiothorac Surg. 27:45-52.
- McBride JT, Wohl ME, Strieder DJ, Jackson AC, Morton JR, Zwerdling RG, et al. (1980). Lung growth and airway function after lobectomy in infancy for congenital lobar emphysema. J Clin Invest. 66:962-970.
- Nakajima C, Kijimoto C, Yokoyama Y, Miyakawa T, Tsuchiya Y, Kuroda T, et al. (1998). Longitudinal follow-up of pulmonary function after lobectomy in childhood - factors affecting lung growth. Pediatr Surg Int. 13:341-345.
- Narayanan M, Owers-Bradley J, Beardsmore CS, Mada M, Ball I, Garipov R, et al. (2012). Alveolarization continues during childhood and adolescence: new evidence from helium-3 magnetic resonance. Am J Respir Crit Care Med. 185:186-191.
- Chong Y, Rhee YJ, Han SJ, Cho HJ, Kang SK, Kang MW. et al. (2016). Life-Threatening Congenital Cystic Adenomatoid Malformation in the Premature Neonate. Korean J Thorac Cardiovasc Surg. 49:210-213.
- Marshall KW, Blane CE, Teitelbaum DH, van Leeuwen K. (2000). Congenital cystic adenomatoid malformation: impact of prenatal diagnosis and changing strategies in the treatment of the asymptomatic patient. AJR Am J Roentgenol. 175:1551-1554.
 Abstract
Abstract  PDF
PDF